Abstract:
An aging population and rising healthcare costs are major issues that the United States is facing today and will continue to face in the future. Medicare and Medicaid, which were developed to provide healthcare for people aged 65 and over, do not cover the needs of oral health maintenance. When it comes to oral health, preventive care is the most critical aspect, especially regular cleaning to avoid caries and periodontal disease. Many dental problems are preventable with good daily mouth care. Problems that are detected early usually are inexpensive and easy to fix.
The insurance system, which was developed to provide healthcare for people aged 65 and over, is not covering their needs for oral health. Preventive care is the most critical part of oral health, especially regular cleaning to avoid caries and periodontal disease. Medicare provides very little coverage for oral health and, even then, only in cases related to services received in a hospital. Medicaid coverage depends on state budgets.(1) With limited income and no insurance, seniors usually skip visiting the dentist, even though many have oral problems such as a dry and painful mouth and difficulty biting and chewing, and many may avoid smiling and decrease their social interaction if they have missing or damaged teeth. Dental problems also impact a person’s overall health, especially if he or she already has a chronic disease.(2)
Determinants of Oral Health
Most people know that poor oral care leads to tooth cavities, but many do not realize that more serious health problems can result from poor oral care. Seniors can face far more serious consequences than a simple toothache or unsightly stains and bad smells from poor oral hygiene. Many elderly people suffer from multiple chronic diseases, such as hypertension, diabetes, arthritis, pulmonary disease, and cancer. The medications taken for these diseases often create dry mouth and, because of this side effect, elderly people are more prone to dental caries or periodontal problems. Dental cavities are not limited to just holes in the tooth and include any type of collection of bacteria in the mouth. If cavities are not treated in time, this collection of bacteria gains access to the bloodstream. Periodontal disease is linked to chronic conditions due to inflammation, and this worsens when a person has existing systemic diseases.(3,4)
According to the Mayo Clinic and the American Dental Association (ADA), concerns related to chronic disease are as follows(5):
Cardiovascular disease: The bacteria from inflammation of the gums and periodontal disease can enter the bloodstream, travel to the arteries in the heart, and cause atherosclerosis. Atherosclerosis causes plaque to develop on the inner walls of arteries, which narrows them and may decrease or block blood flow through the body. This increases the risk of a heart attack or stroke. The inner lining of the heart also can become infected and inflamed, a condition known as endocarditis. Endocarditis can lead to the entire heart becoming inflamed, a life-threatening condition.(6)
Dementia: The bacteria from gingivitis may enter the brain through either nerve channels in the head or the bloodstream, which may lead to the development of Alzheimer disease. Alzheimer disease, the leading cause of dementia, affects more than 5 million Americans and is the sixth leading cause of death in the United States, according to the Alzheimer’s Association.(7)
Diabetic complications: Inflammation of gum tissue and periodontal disease can make it more difficult to control blood sugar and worsen the symptoms of diabetes. Persons with diabetes are more susceptible to periodontal disease, making proper dental care even more important for them.(8)
Respiratory infections: Breathing in bacteria from the infected teeth increases the chances of aspiration pneumonia.
Poor oral care also can affect the immune system, bone strength, and joint disease.
Psychosocial Effects
Poor oral health is not limited to physical effects: it affects elderly people psychologically as well. Some of these psychological issues include the following problems:(9)
Pain and difficulty with eating can lead to poor levels of nutrition and can debilitate aging people.
Some medications taken by older people may cause a dry mouth, which can affect appearance and lead to difficulty in speaking and eating.
Poor appearance and dental incapacity can lead to low self-esteem and social isolation, which may lead to depression.
It is commonly accepted that people should smile in job interviews, and that employers are less likely to hire people with missing teeth, especially for jobs that entail interacting with the public. Many low-income adults have missing or damaged teeth. More than one-fourth (29%) of low-income adults report that the appearance of their mouth and teeth affects their ability to interview for a job. Low-income adults are twice as likely to have this problem as higher-income adults. Employers fear that employees with dental problems will miss workdays or be less productive. In 2008, more than half of U.S. Army recruits were classified as nondeployable unless they got treatment for urgent dental conditions that would likely cause a dental emergency within 12 months.(10)
Dental Insurance
Dental insurance is a form of insurance coverage purchased to reduce the consumer’s out-of-pocket share of costs associated with dental care. Coverage differs from one dental plan to another. Senior citizens may be able to access the following types of dental insurance:
Medicare: Medicare does not provide dental coverage, which means that people over 65 who take part in the program must pay out of pocket for preventive and other dental care. Medicare coverage is limited to medically necessary treatment, such as dental extraction during transplantation, heart valve replacement, preparation for radiation therapy, or jaw reconstruction after an accident. It does not cover routine or preventive dental care, except through Medicare Advantage, which includes vision, dental, and prescription drug coverage. Supplemental Medicare plans can be purchased through private insurance companies under federal guidelines.(1)
Medicaid: Medicaid, the federal/state program for low-income citizens, may cover some dental care for adults, but benefits vary by state, and only 20% of dentists nationwide accept Medicaid.(11)
Commercial insurance: Dental insurance plans for seniors are sold by commercial or private insurance companies and do not need to be coordinated through Medicare. Most plans have a separate premium, but stand-alone plans can be considered affordable for the coverage they provide. The type and level of coverage provided by these plans depends on the premiums.
Out-of-pocket: When people pay money out-of-pocket for the care they received, is known as self-pay. According to 2013 data from the ADA, which surveyed private dentists, the average cost of a basic examination was about $45, and the cost of a cleaning was $85. X-rays were another $27; and a tooth-colored filling was $149, whereas a silver filling was about $125. Costs vary widely depending on the market.(12)
Oral Health Needs of Older Adults
The elderly population has more oral care needs than any other demographic in the United States. According to the ADA, with aging, the nerves in the teeth become smaller, cavities increase, and other health problems can go undetected for a longer time.(13) This makes visiting dentists regularly more important. Some issues include the following:
Dental caries and cavities: When people age, their gums begin to recede. The roots of the tooth are exposed, and it is very easy for cavities to develop in these areas. Cavities can lead to infection and teeth breaking off. A yearly visit to the dentist is a good preventive measure.(14,15)
Gum disease: Plaque grows on the surface of the teeth. The bacteria found in plaque produces acids that cause gum disease. To prevent gum disease and decay, individuals need to remove plaque daily by brushing and flossing their teeth. The dentist or dental hygienist can demonstrate how to brush and floss correctly. According to the ADA, oral health examination and cleaning should be done every six months.(14,15)
Dry mouth: Older people sometimes produce less saliva. Saliva is a natural mouth protector: it limits the growth of bacteria, cleanses the mouth of food, and bathes the teeth with protective minerals. A reduction in saliva, which results in dry mouth, can lead to dental decay. Dry mouth also can be caused by some diseases, cancer therapy, or medications such as diuretics, antihistamines, anti-anxiety drugs, antidepressants, alcohol, certain bladder medications, and other drugs that slow the flow of saliva.(14,16)
Poor-fitting dentures: Dentures need to be checked and refitted on a regular basis, because they can become loose or uncomfortable. Poor-fitting dentures may drop when a person speaks, and they can cause chewing problems that can lead to poor nutrition.(16,17)
Oral cancer screening: Oral cancer includes cancers of the mouth, throat, tongue, and lips. If you notice red or white spots, sores in the mouth, or bleeding that does not disappear within two weeks, an appointment with a dentist or physician is strongly indicated. These could be early signs of oral cancer.(14,16,18)
Additional Considerations
In the past, most elderly people wore dentures. Now, senior adults are more likely to have their own teeth: this trend opens the door to more complex dental concerns. According to the ADA, “In the past, you didn’t have to deal as much with periodontal disease, tooth decay, infection, amputated crowns, and things like that.”(18)
The federal government estimates that 70% of seniors lack dental insurance.
Another modern issue is that up to 88% of all seniors take at least one medication, and most of these medications affect salivary flow. Hundreds of commonly prescribed medications, including those used to treat hypertension, arthritis, depression, and Parkinson disease, can cause xerostomia, or dry mouth, which puts people at higher risk for tooth decay.
The federal government estimates that 70% of seniors lack dental insurance. That is significant, because research has shown that seniors who do have dental coverage are far more likely to go to the dentist. A 2013 report from Oral Health America (OHA) presents a gloomy picture of the overall oral health of the nation’s senior citizens, as reflected in the report’s title, “A State of Decay.” Contributing factors, the report says, are the lack of adult dental benefits through Medicaid programs in almost half the states and dental workforce shortages in almost two-thirds of the states.(18)
About 10,000 Americans retire every day. With retirement often comes the loss of workplace benefits, including dental insurance. Dental coverage is not provided under Medicare, and supplemental private policies are often expensive. Most elderly people procrastinate or avoid dental treatment due to financial constraints. With limited sources of income and Social Security, senior adults prefer to spend on more necessary items. Most of them are not even aware of the impact of oral health on general health. Adults go to primary care settings for their annual checkups and drug refills. Better coordination between oral and general healthcare could improve the overall health of our aging population.(18)
Assessment of Oral Care in the Primary Setting
According to two former U.S. Surgeon Generals, oral disease is a silent epidemic affecting some of our most vulnerable citizens: children and elderly persons.(19) Providing oral healthcare to people throughout their lives improves individuals’ economic well-being as well as their overall physical and psychological health. Integrating oral health with general health can improve the health of the community. Checking oral health status in the primary care setting and providing dental health referrals can improve the quality of life of elderly people. These interventions include:
Decreased emergency visits: People with severe pain from oral health conditions often end up in emergency departments (EDs), where they get drugs for their pain, such as opioids, and antibiotics, rather than complete care. This is costly and ineffective. Studies show that ED-related dental visits significantly increase when elderly people do not get proper dental care.(20) In 2012, emergency dental visits cost the U.S. healthcare system $1.6 billion. The ADA estimates that up to 79% of ED dental visits could be diverted to community settings, saving about 48% of the cost of each visit. For example, treating a dental emergency might cost $750 in an ED, whereas it would cost $390 in the community setting. Encouraging primary care providers to refer patients to dentists can reduce healthcare costs.(21)
Chronic disease management: Four recent studies have analyzed the insurance claims of people with chronic diseases linked to oral health, such as diabetes, congestive heart failure, asthma, chronic obstructive pulmonary disease, coronary artery disease, and chronic kidney or renal disease. All four studies found that overall medical costs were lower for people who received periodontal treatment and cleanings.(20)
Getting old and eating healthy foods: Among people 65 and older with incomes under $15,000, nearly three out of five people have lost six or more of their teeth. More than one in four have lost all of their teeth due to decay or gum diseases. Because they can no longer chew properly, many elderly people cannot eat fruits and vegetables, and many are on soft diets. Unfortunately, soft food can cling to the gums and remaining teeth, further aggravating problems.(22)
Early diagnosis of other disease: Research shows that diseases such as diabetes, leukemia, HIV/AIDS, some cancers, heart disease, and kidney disease have oral manifestations. Besides causing pain and difficulty eating, poor oral health can lead to problems with the heart and other organs.(20)
Strategy to Improve Dental Care for Older Americans
The large numbers of diseases attributed to poor oral health has been labeled a “silent epidemic” by the U.S. Surgeon General.(19) Oral disease is one of the most preventable diseases and presents a challenge for today’s healthcare providers. Unfortunately, this preventable disease is still prevalent among the most vulnerable populations, including seniors, children and adolescents, low-income people, minority groups, and people with special healthcare needs. Inadequate oral healthcare access can lead to advanced oral disease, compromised health status, and, occasionally, even death.(1) The increasing number of older Americans and the persistent barriers they encounter to access and the utilization of services has increased interest in oral health among primary healthcare providers. This has compelled healthcare workers to think of new ideas to overcome the problems facing older Americans and improving the health of people.
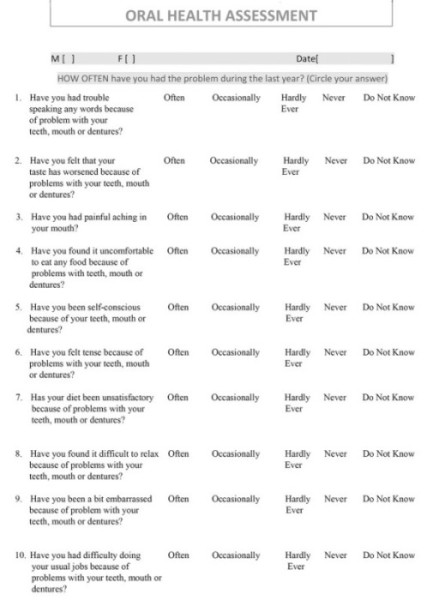
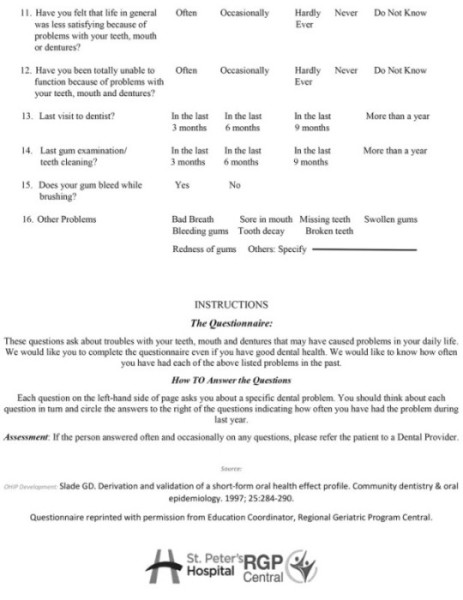
Early treatment for dental disease is the key to prevention. The use of oral health assessment in primary care will help to mitigate acute and chronic health problems. Most seniors have a fixed and limited income, which forces them to view oral health secondary as to physical health. Most Federally Qualified Health Centers, where these seniors usually go for their healthcare needs, do not provide dental services.(4) Assessments of oral health in the primary care setting by primary care doctors can let patients know that they need to visit a dental provider. This will encourage access to treatment before dental problem become more acute. To conduct the assessment, patients will fill out a questionnaire, which includes questions about their oral health and status, while waiting for the provider in the waiting room (Figure 1). It is important to give appropriate training to nurses or physicians about the questionnaire and its assessment properties so they can explain it to the patients and refer them for dental care as needed. This questionnaire has been used in Australia, the United Kingdom, and Canada to assess the oral health status of the adult population.(23) As Americans have a similar lifestyle, culture, and socioeconomic status, use of this questionnaire is encouraged in the primary care setting to:
Increase the effectiveness and efficiency of both dental and medical professionals in preventing disease, thereby reducing a large number of preventable dental conditions, which are far too often treated in emergency rooms.(24)
Improve chronic disease management and prevention.(20)
Address significant oral healthcare access issues by expanding entry points into the dental care system, especially for at-risk and underserved populations.(25)
Facilitate the use of interdisciplinary techniques to overcome patient-specific barriers to accessing services, such as patient apprehension and anxiety about visiting the dentist.(26)
Provide significant cost savings to the healthcare system by controlling for and reducing risk factors common to dental disease and various chronic diseases, such as diabetes.(27,28)
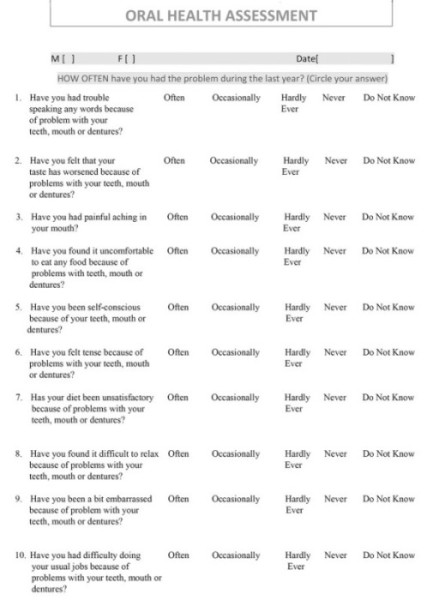
Figure 1. Oral health assessment questionnaire (continues below).
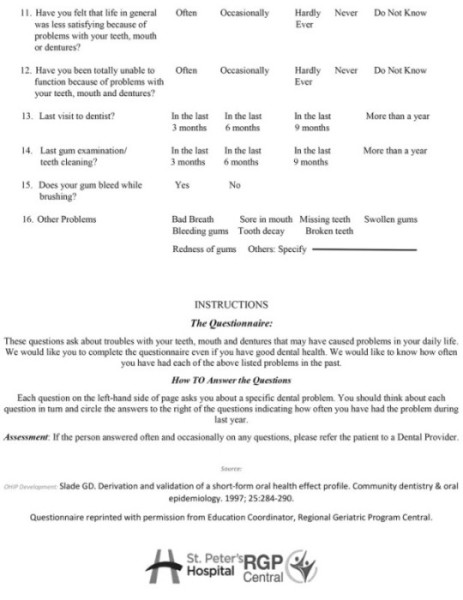
Figure 1 (continued). Oral health assessment questionnaire.
Conclusion
Health insurance coverage in the United States does not meet the basic oral care needs for senior citizens. The older population currently accounts for almost 20% of the U.S. population, and most of them depend on Medicare. Aging-related statistics project that by the year 2030, the number of U.S. adults 65 years or older will reach 72 million, representing 20% of the total U.S. population, which is an approximate doubling in number as compared to the year 2000.(15) By integrating oral healthcare with general healthcare and performing an early assessment of oral problems in the primary setting, the overall health of the elderly population will improve.
Focusing on general health and oral health in the primary setting is cost-effective, eliminates excruciating and unnecessary mouth pain, increases the likelihood of catching oral disease before it worsens, improves a people’s ability to eat and obtain good nutrition, helps adults get jobs, and improves overall health.
References
Center of Healthcare Strategies. Strategies to improve dental benefits for the Medicaid expansion population. www.chcs.org/media/CHCS-Revised-Adult-Dental-Benefits-Brief__021214.pdf . Accessed February 2017.
For seniors, teeth need care—but insurance coverage is rare. http://daily-retirement.com/for-seniors-teeth-need-care-but-insurance-coverage-is-rare/. Accessed October 16, 2016.
Demmer RT, Desvarieux M. Periodontal infections and cardiovascular disease: the heart of the matter. JADA. 2006;137(Supplement 2):14S-20S.
Jaffe S. Seeking dental care for older Americans. Health Aff (Millwood). 2016;35:2164-2167.
Oral health: a window to your overall health. www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475 . Accessed April 30, 2017.
Systemic diseases caused by oral infection. http://cmr.asm.org/
content/13/4/547.full. Accessed May 5, 2017.A link between gum disease and Alzheimer’s? www.medicinenet.com/script/main/art.asp?articlekey=174327 . Accessed October 2016.
Periodontal disease and diabetes. www.ada.org/~/media/ADA/Member%20Center/FIles/Perio_diabetes.ashx . Accessed October 2016.
Department of Health and Human Services. Effects on well-being and quality of life. www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/sgr/chap6.htm . Accessed May 10, 2017.
Moss D. The 2008 Army Recruit Oral Health Survey Results. US Army Medical Department Journal. 2011;January-March:62-67.
Medicaid adult dental benefits: an overview. www.integration.samhsa.gov/clinical-practice/Adult-Oral-Health-Fact-Sheet_21915.pdf. Accessed on May 10, 2017.
Carrns A. Long-in-the-tooth dental advice. www.nytimes.com/2014/11/19/your-money/long-in-the-tooth-dental-advice-.html . Accessed May 3, 2017.
American Dental Association. Aging and dental health. www.mouthhealthy.org/en/az-topics/a/aging-and-dental-health . Accessed on May 3, 2017.
American Dental Association. Statement on regular visit. www.ada.org/en/press-room/news-releases/2013-archive/june/american-dental-association-statement-on-regular-dental-visits . Accessed April 10, 2017.
Centers for Disease Control and Prevention. Oral health for older Americans. www.cdc.gov/oralhealth/publications/factsheets/adult_oral_health/adult_older.htm . Accessed April 3, 2017.
American Dental Association. Aging and dental health. www.ada.org/en/member-center/oral-health-topics/aging-and-dental-health . Accessed April 20, 2017.
American Dental Association. Removable partial denture. www.mouthhealthy.org/en/az-topics/d/dentures-partial . Accessed on April 3, 2017.
Association of Healthcare Journalist. State of decay in oral health of elderly varies widely by state. http://healthjournalism.org/blog/2016/05/state-of-decay-in-oral-health-of-elderly-varies-widely-by-state/ . Accessed May 31, 2016.
Department of Health and Human Services. Oral Health America: a Report of the Surgeon General. www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/Report/ExecutiveSummary.htm . Accessed April 2, 2017.
Jeffcoat RL, Gladowski PA, Bramson JB, Blum JJ. Impact of periodontal therapy on general health: evidence from insurance data for five systemic conditions. Am J Prev Med. 2014;47(2):166-174.
ADA Health Policy Institute. Emergency department use for dental condition continues to increase. www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0415_2.ashx. Accessed April 5, 2017.
Santa Fe Group. Analysis of data from 2014 Behavioral Risk Factor Surveillance System data, presentation. Oral health inequality in American older adults. Denta Quest Foundation. 2016.
Slade GD, Nuttall N, Sanders AE, Steele JG Allen PF, Lahti S. Impacts of oral disorders in the United Kingdom and Australia. Br Dent J. 2005;198:489-493. doi: 10.1038/sj.bdj.4812252.
Pew Center on the States. A costly dental destination: hospital care means states pay dearly. www.pewtrusts.org/~/media/assets/2012/01/16/a-costly-dental-destination.pdf. Accessed May 1, 2017.
Institute of Medicine (IOM) and National Research Council (NRC). Improving Access to Oral Health Care for Vulnerable and Underserved Populations. Washington, DC: National Academies Press; 2011.
Munger RL, Buncombe County Human Services Support Team. Evolving oral health models: lesson learned from behavioral health. Presentation at the Grant Makers In Health: Returning the Mouth to the Body: Integrating Oral Health and Primary Care. Washington, DC, April 17, 2012. https://www.gih.org/files/FileDownloads/Returning_the_Mouth_to_the_Body_no40_September_2012.pdf .
Cigna. Improved health and lower medical costs: why good dental care is important, Whitepaper. www.cigna.com/assets/docs/life-walllibrary/Whygooddentalcareisimportant_whitepaper.pdf . Accessed May 3, 2017.
Cigna. Medscape publishes Cigna study supporting association between treated gum diseases and reduced medical costs in individuals with diabetes. http://newsroom.cigna.com/NewsReleases/medscape-publishes-cigna-study-supporting-association-between-treated-gum-disease-and-reduced-medical-costs-in-individuals-with-diabetes.htm. Accessed May 3, 2017.