Burnout has received international attention since being independently described by Drs. Freudenberger and Maslach decades ago.(1) Burnout is a known consequence of performing human service work and manifests as emotional exhaustion, cynicism, and low sense of professional achievement.(2-5) Recognizing the detrimental effects of burnout, all European Union member states have passed legislation requiring companies to monitor psychological well-being in the workplace.(6) It is well-established that increasing engagement reduces burnout, but reducing burnout does not improve engagement.(6,9-12)
A recent National Academy of Medicine report suggests six specific goals to help organizations combat burnout.(7,8) Three of their recommendations do not require expensive investments or whole-system transformation. The report encourages organizations to create a positive work environment and a positive learning environment, and provide support to clinicians and learners.
Nevertheless, despite significant system-level and individual-level efforts, burnout rates continue to increase, and work-life balance, exacerbated by COVID-19, continues to decrease.(13-15)
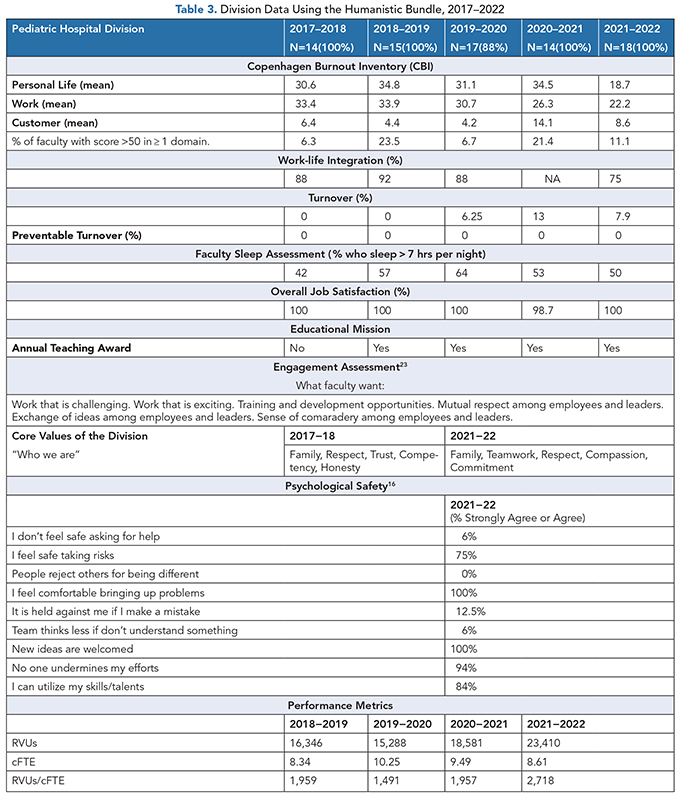
In 2015, our division of 15 pediatric hospitalists began using a bundle of surveys to assess the impact the work climate had on job satisfaction and burnout as a way to better understand what activities were valuable to staff members’ professional and personal satisfaction. Currently, the bundle includes a burnout assessment, an engagement assessment, a division-specific job satisfaction survey, a division leadership 360-degree evaluation, a work-life balance assessment, and an assessment of psychological safety(16) (Table 1).
We conducted a retrospective review of our division’s burnout data over the same time period reported in a recent COVID study.(13,15) Interestingly, burnout and work-life balance trends in our division do not mirror national trends (Tables 2 and 3). This raises the possibility that our division has achieved some of the individual, work unit, and specialty-specific goals that are recommended to improve physicians’ engagement and reduce burnout.(7,8,17,18)

The purposes of this article are four-fold: (1) to discuss the scales used in the Humanistic Bundle and the evidence supporting their use; (2) to outline our process of administering the bundle throughout the employee life cycle; (3) to challenge the existing mental models of interpreting burnout and engagement scores; and (4) to demonstrate how incorporating the bundle’s results with traditional performance metrics provides a holistic and ultimately more accurate assessment of work-unit performance balanced with staffs’ perception of their work climate.
The Humanistic Bundle
Since physician burnout is estimated to affect 35–54% of practicing physicians and 45–60% of resident physicians, it has been compared to a public health crisis.
Conducting burnout assessments without identifying the individual and the problem is similar to screening for cardiovascular disease risk factors without knowing which patient has hypertension, new onset diabetes, or hypercholesterolemia.
Just as patients require individualized medical interventions, so do faculty members. Anonymous burnout assessments are limited by the false assumption that the causes of burnout are identical for everyone. Interventions built on anonymous assessment can only generate unit-level interventions rather than individualized ones. This would be like a clinic prescribing all patients who screened positive for cardiovascular disease the same blood pressure and cholesterol-lowering agents.
Since burnout and disengagement require understanding at the individual level, identifiable assessments generate individual-level interventions. Identifiable data also encourage faculty to be part of the dialogue, reflect on why they answered certain questions the way they did, then propose countermeasures intended to address the problems that generated their burnout score. The leader should support practical, individual-level proposals and monitor for the emergence of division-level themes to determine if a division-level intervention is warranted.
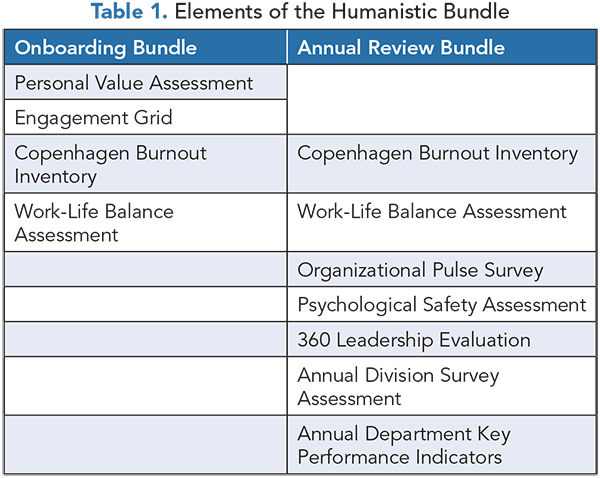
In 2019, after several years of assessing and monitoring faculty burnout, engagement, work-life balance (WLB), and leadership performance, one of the authors (MB), a physician-leader of a clinical division, decided to assess and monitor burnout. He coined the term “Humanistic Bundle” to describe the assessment (Figure 1).
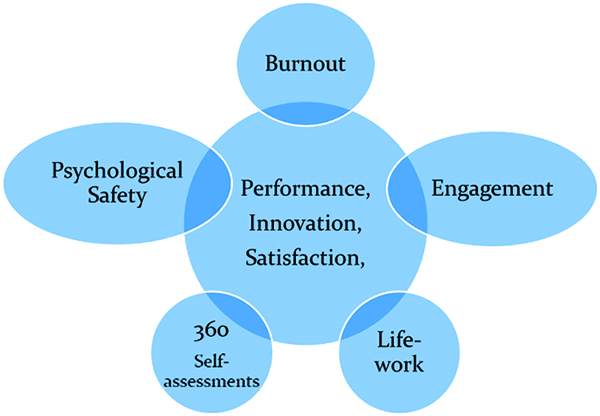
Figure 1. The Humanistic Bundle
The division agreed to participate in a universal screening process similar to that used by primary care providers to screen for modifiable risk factors for cardiovascular diseases that cause stroke, heart attack, and death. The information collected by the bundle is as actionable as medical risk assessments that estimate patient risk for stroke, except that burnout manifests as poor employee retention, under-performance, and interpersonal conflicts.
The Scales of the Humanistic Bundle
1. Burnout
We utilized the Copenhagen Burnout Inventory (CBI), which was validated in the PUMA Study,(5,19,20) a five-year study of 2,391 employees in the human service industry, including physicians. The CBI assesses burnout across three domains: personal, work, and customer-related. A score that exceeds 50 points in any one domain is indicative of burnout.
Although the Maslach Burnout Inventory (MBI) is the most widely used scale, it does have limitations. Primarily, cynicism is a coping strategy of humans within a system, and reduced professional achievement is a consequence of burnout. Measuring cynicism, exhaustion, and low sense of achievement is important, but those factors are secondary to knowing what causes them. Additionally, the CBI measures personal burnout, which is not measured by the MBI. Finally, since the PUMA study categorized determinants and consequences of burnout among physicians, the Copenhagen Inventory presented itself as a rational alternative to the MBI.
2. Job Satisfaction and Work-Life Balance
To assess job satisfaction and work-life balance (WLB), we asked faculty to answer three questions. First, we asked them to rate their overall satisfaction with clinical duties using “very satisfied,” “satisfied,” “neutral,” “dissatisfied,” and “very dissatisfied” as measurements. Respondents who answered “very satisfied” or “satisfied” were deemed satisfied.
The second question assessed the average number of hours of sleep per night as “greater than seven hours” or “less than seven hours.” Sleep is assessed because of established correlations with performance, safety, and professional behaviors.(21,22)
Finally, WLB was assessed using the validated question “My work schedule leaves me enough time for my personal/family life.” The response options were “strongly agree,” “agree,” “neutral,” “disagree,” and “strongly disagree.” WLB was defined as “strongly agree” or “agree.”(15)
An added benefit of using the Copenhagen inventory is that it also assesses WLB in the “work-related burnout” domain with the question, “Do you have enough energy for family and friends during leisure time?”
3. Engagement
At the organizational level, engagement is measured every two years using a Pulse Survey. This anonymous 43-question survey assesses five domains: engagement, alignment, safety, resilience, and diversity. Engagement is a composite metric consisting of six items that measure employees’ degree of pride in the organization, intent to stay, willingness to recommend, and overall workplace satisfaction. The Pulse Survey can provide only department-level and occasionally division-level data.
In addition to the Pulse Survey, faculty were asked to complete a 4 × 3 engagement grid. The grid was constructed from the Human Capital Institute’s survey that assessed the 12 characteristics of an engaging work climate.(17) Faculty were asked to check the three most important attributes of a desirable culture and work climate. Debriefing sessions required faculty to describe what these characteristics meant to them and how the characteristics could be incorporated into the work space. This grid has been incorporated into new faculty onboarding (Table 1).
4. The 360-degree Evaluation
The scale was adapted from an assessment scale published in the Institute of Healthcare Improvement’s Improving Joy in Work.(20,23) The scale includes 13 items asking respondents to assess their local leader using a 5-point scale. It also poses two open-ended questions: one asking how a leader can improve and a second asking about the leader’s perceived strengths.
The survey is distributed to faculty via email using Survey Monkey® one month ahead of their annual performance reviews. Data are collected anonymously. All scores and comments are incorporated into MB’s annual report that is submitted to the department chair.
5. Values Assessment
The presence of shared values among team members improves engagement, reduces burnout, and enhances performance.(8,20,23) The Humanistic Bundle also assesses faculty values. Faculty are asked to select their top five values from a list of 30. Self-determination theory (SDT)(24) and Expectancy Theory(25-27) are two motivational theories that describe how values are incorporated in decision-making. These complimentary theories explain why teams that understand their values cultivate personal growth, pride, and commitment in the workplace.(8,24) When physicians can articulate their personal and professional values, they can better prioritize their days’ agenda and their career goals.
Physicians are increasingly asked to complete more tasks within fixed work hours. As such, they are required to make more decisions per day, which stretches their cognitive bandwidth and results in cognitive scarcity — a feeling of not having the cognitive capacity necessary to perform well.(28) As a result, physicians use discretionary effort based on how much they expect their effort will result in improved performance and better outcomes. The caveat is that people will not work harder if the outcome or the incentive isn’t valued.(29)
When faculty members who understand their values are presented with career opportunities and incentives, they can prioritize their efforts better and pursue activities they find most engaging and in alignment with core values. Additionally, pursuing “non-value-added” activities can result in internal strife, cynicism, discontent, disengagement, inter-personal conflict, and turnover.
6. Psychological Safety
Amy Edmondson described psychological safety in her book The Fearless Organization(16) as “the belief that a work environment is safe for interpersonal risk taking” and as feeling free to surface ideas, questions, or concerns.(16) She discovered that safety can be shaped by local leaders; thus, its presence often varies across organizations. It is not simply about being nice or showing trust or being willing to lower performance standards.(16) Psychological safety correlates with learning behaviors, divergent thinking, information-sharing, and problem-solving while maintaining high performance standards.
We began assessing psychological safety as a scale of the Humanistic Bundle in 2021. However, given that high levels of psychological safety among faculty is critical when asking them to complete scales in an identifiable manner, it might be important to assess this metric anonymously before conducting other assessments.
The Implementation Process
Rolling out implementation of the Humanistic Bundle requires a clear communication plan that explains the bundle’s purpose, why certain scales are used, and why some scales are identifiable and others are anonymous. The rollout should emphasize the importance of being honest and professional when offering and receiving feedback.
Leaders might consider incentivizing group participation; however, they should not offer physicians financial incentives to demonstrate a reduction in burnout. Incentivizing results as opposed to honest participation can lead to surrogating or gaming behaviors among respondents, which could conceal worsening burnout or disengagement rather than identify it.
This exercise requires two bundles tailored to two specific circumstances. One bundle is part of new-faculty onboarding and a second is part of the annual “stay interview” process (Table 1). Because all employees have a lifecycle that starts with recruitment and ends with an exit, our process follows the Human Performance Management Cycle(30) (Figure 2).
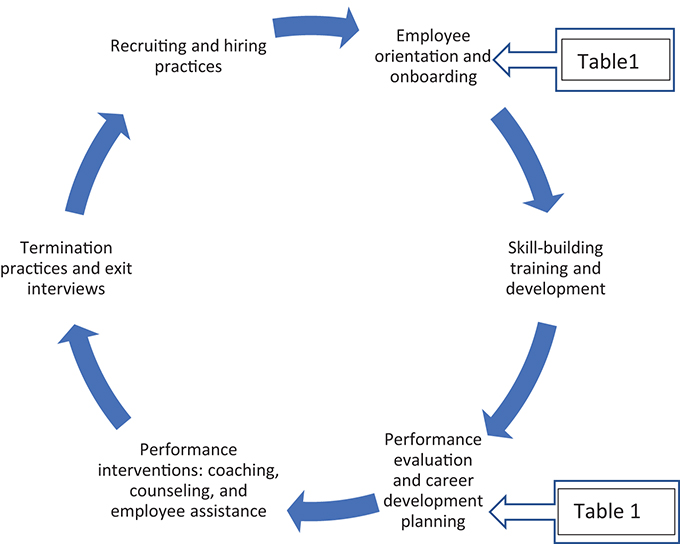
Figure 2. Overview of Human Performance Management Cycle(30)
Because the bundles must accommodate new and existing faculty, the scales in the “onboarding bundle” differ slightly from those included in the “annual review bundle.” For example, the onboarding bundle includes a baseline burnout assessment, an engagement grid, a personal values assessment, and WLB assessments, but not a 360-degree evaluation. Screening during onboading permits assessments of graduating residents or “at-risk” physicians recruited from other health systems, because they likely are experiencing some degree of burnout or disengagement.
Baseline data serve as historical controls that permit longitudinal tracking of scores over time. This method quantifies the positive or negative effects the system has on faculty through comparison of subsequent scores to baseline scores. Because the scores are indentifiable, this approach also makes it possible to test the effectiveness of individual-level interventions over time.
Synthesizing The Bundle
This section highights several distinct features of complex adaptive systems and explains how these features limit our ability to interpret burnout and engagement using traditional analysis. Additionally, we describe the two types of problems all leaders face working in a complex system. Finally, we highlight the importance of developing new leadership competencies to administer the bundle.
First, engagagement and burnout data are not like other performance indicators measured in healthcare, such as RVUs or length of stay. Burnout and engagement are byproducts of multiple interactions between people working in a complex system and are best understood as non-linear, emergent properties.
Linear quantities exhibit forward causality, have only one solution, are predictable, and collecting more data makes a problem more solvable. However, because emergent properties are non-linear quantities, they exhibit multidirectional causality, are anticipated versus predictable, and are not readily solved by collecting more data.(31) Other real-world examples of emergent properties are love, trust, cynicism, and high-performance.
Focusing on high-performance, what leads to one team becoming a high-perfoming team and not another, despite each team’s members possessing equivalent skills and training? High-performing teams often exceed expectations and exhibit trust, credibility, respect, fairness, pride, and comradery.(32) High performance is often achieved because of how a coach manages the interactions between players, not the actions of the players.
Burnout and high performance are both emergent properties. Measuring burnout is easy, but managing it is difficult because it is a byproduct of so many interactions in a system and because it emerges over time. Therefore, engagement and burnout are unlikely to be solved by simply adding resources or subtracting demands.
Second, although burnout and disengagement are considered to be problems, they should be conceptualized as symptoms of problems. There are two general types of problems: ill-structured and well-stuctured problems.(33) A well-structured problem applies rules, principles, and concepts, and if enough data exist, the problem can be solved. An ill-structured problem lies at the other end of the contiuum and is not solved by simply acquiring more data or applying a better algorithim.(33) Studies have shown groups that have solved ill-structured problems were multi-disciplinary, used different ways of processing information, communicated differently, and generated several alternative solutions.(33)
For example, diagnosing the cause of shortness of breath as a pulmonary embolism represents solving the symptoms of a well-structured problem. Physicians conduct a history and a physical, and order laboratory and radiologic studies to make the diagnosis. However, managing a pulmonary embolism in a patient with renal failure, no insurance, swallowing difficulty, and transportation insecurities represents an ill-structured problem. The first example, a well-structured problem, has one right answer; the second example has many partial solutions. Perhaps little progress has been made in burnout because we are treating it as a linear, well-structured problem as opposed to emergent symptoms of ill-structured problems.
Finally, since burnout and disengagement emerge from ill-structured problems, addressing them requires new ways of processing the information and adopting a growth and development coaching mindset. There are two types of coaching: perfomance coaching and growth and development coaching.(34)
Perfomance coaching is a familiar model. It is a deficit-facing, past-focused approach that uses performance data. Conversely, growth and development coaching is an asset-facing, possibility-focused, inclusive approach that uses conversations to identify strengths, interests, and values to improve performance. Leaders who use a growth and development coaching approach encourage individuals to come up with their own ideas for change by using their strengths in ways that align with core values.
Both models are vital, but growth and development coaches use appreciative inquiry,(35) positive psychology,(36) and learning behaviors(37) to build the engaged, high-peforming teams needed in today’s dynamic healthcare environments.(38) Leadership styles needed to achieve this are often considered transformational, situational, and servant-based; they intentionally use path-goal and leader-member exchange theories.
The Conversation
Implementing the Humanistic Bundle in an identifiable manner allows leaders to share results with each respondent in one-on-one conversations and apply performance and development coaching. In these coaching sessions, each faculty member is given the opportunty to explain why they answered certain questions the way they did. They are also given the opportunity to suggest what they think they need to meet personal and professional goals. Sessions that occur in an identifable manner can generate person-specfic interventions that can’t be accomplished using aggregate data.
Development coaching can reduce the “learned helplessness” seen in cynical, burned-out people and replace it with a sense of agency and self-helpfulness. If the leader supports a suggested intervention, the success of the internvention will be reflected positively in scales of the bundle and performance metrics. If an intervention is less successful than anticipated, then that too will become evident. This approach replaces assumptions made regarding the causes of employee disengagement with credible information. Finally, this approach creates feedback loops between the leader-respondent dyads and creates a positive learning environment.
Our annual reviews now routinely incorporate the Humanistic Bundle with traditional key performance metrics. All faculty members complete the leader 360 evaluation and job satisfaction survey, Copenhagen Burnout Inventory, and psychological safety evaluation ahead of their annual reviews. Data are compared year-to-year so the team can assess and discuss the effect of the system on burnout and the effectivess of past interventions. This allows the team to engage in conversations around performance, system demands, and how to achieve goals. Growth and development coaching helps faculty reframe the negative elements captured by the bundle more positively by discussing practical goals plans to achieve them rather than perseverate on a score.
Once all of the individual annual reviews are completed, the data are de-identified and shared at the division meeting. During this meeting, faculty can see the division’s clinical productivity, scholarship, and educational achievements. Additionally, each faculty member can see all of the data collected by the Humanistic Bundle, which includes the leader’s 360 evaluations and the team’s psychological safety profile. This approach engages the collective intelligence of the team by inviting and challenging them to interpret the data. This approach has led to re-interpretation of some of the results and division-level interventions generated by the team.
Sharing the 360 evaluation can be uncomfortable for the leader, but it is a vital part of the process. It demonstrates vulnerability and humility and pays dividends in building trust and safety among the team.
Results
Our data demonstrate several things. First, burnout and WLB measurements conducted on physicians in our divison do not mirror national data (Tables 1 and 2). This could be because of using different burnout assessment instruments, which limits comparison with other studies that employ the Maslach Burnout Inventory. While comparison in raw scores isn’t possible, the trends remain informative and are reflected in high retention rates and clinical performance.
Work-life balance in our group is greater than double the national rates using the same assessment question despite decreasing cFTE and increasing clinical productivity (Table 3). Our data also show that personal exhaustion peaked during COVID-19, but has since returned to pre-COVID-19 levels. Interestingly, work-related and customer-related burnout remained stable throughout the pandemic. During the pandemic, there was an increase in the number of faculty who had a burnout score that exceeded 50 points in at least one domain; however, this returned to pre-pandemic levels.
The customer/patient domain consistently represents an area with the lowest burnout scores, suggesting that physicians in our division are not burned out because of treating patients. This is supported by job satisfaction scores of 100% and preventable physician turnover of 0% (Table 3). Because our division conducts exit interviews, we know that the six faculty who left during this period left for family reasons and not because of job disatisfaction or burnout. They all said “yes” to the question “If circumstances allowed, would you come back to work for the division?”
A possible explanation for the aggregate reduction in burnout scores (Table 3) could be new faculty who had lower burnout scores than the faculty they replaced. WLB did decrease during the pandemic, but not to the levels reported nationally (75% vs. 30%, respectively).
The data can be interpreted by using a group’s collective intelligence. After reviewing the data, team members hypothesized that WLB decreased because of excess work-life integration. They speculated that WLB was negatively affected during the pandemic because of the implementation of multiple modalities to contact physcians who were increasingly working remotely. Our team believed this encroached on WLB because no rules of engagement were developed about contacting physicians. This led to frequent interruptions, difficulty disengaging from work, and parodoxically, getting engaged in work.
While it was generally agreed that remote work had benefits, it blurred prexisting work-life boundaries. WLB was impaired because of frequent school and daycare interruptions, which made it difficult for faculty to complete work from home while simultaneously trying to care for young children. Despite these challenges, WLB in our division averaged 86% compared to 40% at the national level (Table 3).
In an academic department of more than 175 physicians, our division is expected to contribute to our health system’s educational mission. Our division’s average resident evaluation exceeds the department’s average, and three members of our division have received annual teaching awards for four of the past five years (Table 3). As an academic division, it was important to us to determine whether burnout and engagement can improve while meeting our commitment to providing mission-critical, albeit non-RV-generating work.
Finally, in terms of organizational citizenship, our division occupies four out of five residency leadership positions and several hospital-level leadership roles. We encourage readers who employ this approach to develop specialty and/work unit-relevant metrics that serve as key performance indicators of a highly engaged team.
Discussion
Our division of 15 pediatric hospitalists at an academic medical center have used the Humanistic Bundle since 2014. Given the discordant rates of burnout and work-life balance reported in our group versus those at a national level, we wanted to share the process of gathering, reporting, and addressing this problem.
We do not assert that our approach solves burnout; rather, we suggest that organizations consider adopting “people-oriented” metrics to complement the traditional “production-oriented” metrics (Table 3). This report is limited by being a retrospective analysis of a small sample size of pediatric hospitalists at a single academic center. Because burnout and disengagement varies across specialites and organizations, this could limit the generalizability of our results.(8) However, given the participative nature of this process, we believe the stay-interviews using data from the bundle conducted as part of our annual review process empowers respondents.
Our approach represents real-world application of organization development practices using self-determination and motivation theories, which are antidotes to cynicsm, low professional achievement, and emotional exhaustion.(25,26,39,40) The process of collecting and reporting 360 leadership feedback helps cultivate psychological safety and trust among the leader and the team. Psychological safety can neutralize the presence of power differentials that might prevent people from answering survey questions honestly, which is why psychological safety is a critical metric of the bundle. Even though this was the last assessment added to our bundle, one could make cogent argument that psychological safety should be the first area assessed. It is possible that our process of collecting and discussing burnout and engagement destigmatizes it and nomalizes conversations.
We believe that our commitment to the Humanistic Bundle and our transparency in reporting contributed to creating a positive work environment and a positive learning environment which provided support to clinicians and learners.
The Humanistic Bundle can be implemented at any level of any organization. Its use might isolate the level of the organization where problems exist, which could facilitate more accurate corrective actions without assuming causality. Larger prospective studies could determine if using the Humanistic Bundle reduces burnout, enhances engagement, or improves psychological safety before broader adoption. Future studies should be designed to determine if use of the bundle improves mission critical metrics.
A recent study calculated the cost-consequence of burnout for organizations that employ ≥1,000 physicians. Results estimated that the average burnout-related costs are $7,600 per employed physician per year (range $3,700-$11,000). Given the time-intensive nature of this approach, it could be argued that it is only feasible to conduct in small work units. However, given the inertia around reducing burnout, perhaps discussions should begin to include whether we can afford to not try new approaches. This intervention incurred zero dollars to employ, so the return on investment seems favorable.
Conclusion
Since 2014, the Division of Pediatic Hospital Medicine has been conducting annual assessments using a Humanistic Bundle. Data from our division indicates that even in the face of COVID and staffing issues, burnout and WLB are stable and have not mirrored the upward trends reported nationally in healthcare.(13) Performance across the missions has been excellent, job satisafction is high, and preventable turnover is zero. Given the inertia around burnout, we believe our approach to measuring it, our conversations about it, and our leadership behaviors must change.
Acknowledgment: The authors acknowledge Drs. J. Aprile, W. Beachy, C. Bridgeman, S. Clarke, A. Daly, C. Daymont, E. Despeux, M. Ilgenfritz, C. Irvin, L. Keefer, P. Kumar, A. Nelson, S. Nguyen, C. O’Hara, A. Schuster, B. Smith, R. William.
References
Borritz M, Rugulies R, Bjorner JB, Villadsen E, Mikkelsen OA, Kristensen TS. Burnout Among Employees in Human Service Work: Design and Baseline Findings of the PUMA Study. Scand J Public Health. 2006;34(1):49–58. https://doi.org/10.1080/14034940510032275
Shanafelt TD, West CP, Sloan JA, et al. Career Fit and Burnout Among Academic Faculty. Arch Intern Med. May 25 2009;169(10):990-995. https://doi.org/10.1001/archinternmed.2009.70
Maslach C, Leiter MP. Understanding the Burnout Experience: Recent Research and Its Implications for Psychiatry. World Psychiatry. Jun 2016;15(2):103–111. https://doi.org/10.1002/wps.20311
Maslach C, Schaufeli WB, Leiter MP. Job Burnout. Annu Rev Psychol. 2001;52:397–422. https://doi.org/10.1146/annurev.psych.52.1.397
Maslach C. What Have We Learned About Burnout and Health? Psychol Health. Sep 2001;16(5):607–611. https://doi.org/10.1080/08870440108405530
Schaufeli WB. Applying the Job Demands-Resources Model: A ‘How to’ Guide to Measuring and Tackling Work Engagement and Burnout. Organizational Dynamics. 2017;46:120–132. https://doi.org/10.1016/j.orgdyn.2017.04.008
National Academies of Sciences, Engineering, and Medicine Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington, DC: National Academies Press; 2019.
Shanafelt TD, Noseworthy JH. Executive Leadership and Physician Well-being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout. Mayo Clin Proc. Jan 2017;92(1):129–146. https://doi.org/10.1016/j.mayocp.2016.10.004
Demerouti E, Bakker AB, de Jonge J, Janssen PP, Schaufeli WB. Burnout and Engagement at Work as a Function of Demands and Control. Scand J Work Environ Health. Aug 2001;27(4):279–286. https://doi.org/10.5271/sjweh.615
Bakker AB, Demerouti E, Euwema MC. Job Resources Buffer the Impact of Job Demands on Burnout. J Occup Health Psychol. Apr 2005;10(2):170–180. https://doi.org/10.1037/1076-8998.10.2.170
Bakker AB, Demerouti E. Job Demands-Resources Theory: Taking Stock and Looking Forward. J Occup Health Psychol. Jul 2017;22(3):273–285. https://doi.org/10.1037/ocp0000056
van Turin L, Schaufeli WB, Van den Broek A. Engaging Leadership: Enhancing Work Engagement Through Intrinsic Values and Need Satisfaction. Human Resource Development Quarterly. 2021;32:483–505. https://doi.org/10.1002/hrdq.21430
Whang O. Physician Burnout Has Reached Distressing Levels, New Research Finds. The New York Times. September 29, 2022.
Author Google Search “Covid, physician burnout” 2022.
Shanafelt TD, West CP, Dyrbye LN, et al. Changes in Burnout and Satisfaction with Work-Life Integration in Physicians During the First 2 Years of the COVID-19 Pandemic. Mayo Clin Proc. Dec 2022;97(12):2248–2258. https://doi.org/10.1016/j.mayocp.2022.09.002
Edmondson A. The Fearless Organization: Creating Psychological Safety in the Workplace for Learning, Innovation, and Growth. 1st ed. New York: Wiley; 2018.
Wiete AK, The Trifecta of Engagement: The Organization, the Manager, and the Employee. Human Capital Institute. 2013:1–36. https://www.hci.org/research/trifecta-engagement-organization-manager-and-employee
Dyrbye LN, Shanafelt TD, Gill PR, Satele DV, West CP. Effect of a Professional Coaching Intervention on the Well-being and Distress of Physicians: A Pilot Randomized Clinical Trial. JAMA Intern Med. Oct 01 2019;179(10):1406–1414. https://doi.org/10.1001/jamainternmed.2019.2425
Shanafelt TD, Boone S, Tan L, et al. Burnout and Satisfaction with Work-Life Balance Among US Physicians Relative to the General US Population. Arch Intern Med. Oct 08, 2012;172(18):1377–1385. https://doi.org/10.1001/archinternmed.2012.3199
Shanafelt TD, Gorringe G, Menaker R, et al. Impact of Organizational Leadership on Physician Burnout and Satisfaction. Mayo Clin Proc. Apr 2015;90(4):432–440. https://doi.org/10.1016/j.mayocp.2015.01.012
Hagger MS. Where Does Sleep Fit in Models of Self-Control and Health Behaviour? Stress Health. Dec 2014;30(5):425–430. https://doi.org/10.1002/smi.2624
Pilcher JJ, Morris DM. Sleep and Organizational Behavior: Implications for Workplace Productivity and Safety. Front Psychol. 2020;11:45. https://doi.org/10.3389/fpsyg.2020.00045
Perlo J, Balik B, Swenson S, Kabcenell A, Landsman J, Feeley D. IHI Framework for Improving Joy in Work. IHI White Paper. Cambridge, MA: Institute for Healthcare Improvement; 2017. https://www.ihi.org/resources/Pages/IHIWhitePapers/Framework-Improving-Joy-in-Work.aspx
Deci EL, Olafsen AH, Ryan RM. Self-Determination Theory in Work Organization: The State of a Science. Annual Review of Organizational Psychology and Organizational Behavior. 2017;41(1):19–43. https://doi.org/10.1146/annurev-orgpsych-032516-113108
Vroom VH. Work and Motivation. New York: Wiley; 1964.
Vroom VH. Motivation in Management. Hamilton, NY: American Foundation for Management Research; 1965.
Vroom VH, Deci EL. Management and Motivation: Selected Readings. New York: Penguin; 1970:399.
Ariely D, Lanier WL. Disturbing Trends in Physician Burnout and Satisfaction with Work-Life Balance: Dealing With Malady Among the Nation’s Healers. Mayo Clin Proc. Dec 2015;90(12):1593–1596. https://doi.org/10.1016/j.mayocp.2015.10.004
Isaac RG, Zerbe WJ, Pitt DC. Leadership and Motivation: The Effective Application Expectancy Theory. Journal of Managerial Issues. 2001;13(2):212–226.
Langdon DB, Whiteside KS, McKenna MM. Intervention Resource Guide: 50 Performance Improvement Tools. San Francisco: Jossey-Bass/Pfeiffer; 1999.
Gharajedaghi J. Systems Thinking: Managing Chaos and Complexity: A Platform for Designing Business Architecture. Burlington, MA: Morgan Kaufmann; 2011.
Burchell M, Robin J. The Great Workplace: How to Build It, How To Keep It, and Why It Matters. New York: Wiley; 2011.
Jonassen D. Learning to Solve Problems. New York: Wiley; 2004.
Bungay Stanier M. The Coaching Habit: Say Less, Ask More & Change the Way You Lead Forever. Box of Crayons Press; 2016.
Orem S, Binkert J, Clancy AL. Appreciative Coaching: A Positive Process for Change. 1st ed. San Francisco: Jossey-Bass; 2007.
Biswas-Diener R. Practicing Positive Psychology Coaching: Assessment, Activities, and Strategies for Success. New York: Wiley; 2010. https://doi.org/10.1002/9781118269633
Edmondson A. Psychological Safety and Learning Behavior In Work Teams. Administrative Science Quarterly. June 1999;44(2):350–383. https://doi.org/10.2307/2666999
Harvard Business Review. HBR Guide to Motivating People. Boston: Harvard Business Review Press; 2019.
Vroom VH. Some Personality Determinants of the Effects of Participation. (Psychology Revivals). New York: Routledge; 2020.
Vroom V. Reflections on the Roots of Self-Determination. Am J Health Promot. Jul-Aug 2013;27(6):TAHP9.

