The Medicare program was established in July 1965 to provide healthcare coverage for Americans 65 and older and expanded in 1972 to include coverage for people with certain disabilities and end-stage renal disease who were younger than 65. Today, the Medicare program consists of four separate parts. Part A provides hospital insurance. Part B provides medical insurance, including provider fees and outpatient services. Part C (Medicare Advantage) allows private insurers to offer coverage that may substitute for traditional Medicare Parts A and B and often Part D, which covers prescription drugs. After nearly 60 years, Medicare now covers more than 68 million Americans, 90% of whom are 65 and older.(1)
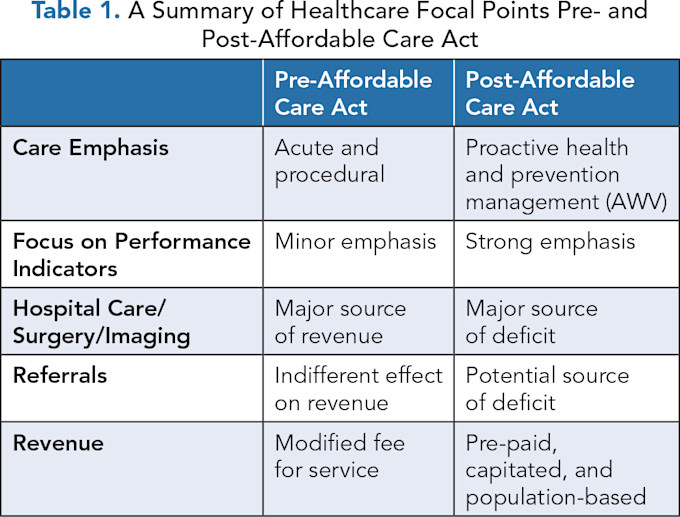
The Patient Protection and Affordable Care Act (PPACA), which celebrates its 15th anniversary in 2025, emphasized moving from a reactive healthcare system focused on illness and disease to one that is proactive and provides people with access to address their physical and mental health.(2) The act also instituted new incentives for physicians and healthcare organizations interested in managing patient populations.(2) Table 1 highlights the differences in focus between pre- and post-Affordable Care Act factors that were conceptualized then and are still relevant today.
THE MEDICARE ANNUAL WELLNESS VISIT
The Medicare Annual Wellness Visit (AWV) resulted from PPACA as an important framework for providing preventive services to Medicare beneficiaries to improve health outcomes and reduce costs.(3–6) This article explores the current state of the AWV, emphasizing its clinical and reimbursement outcomes for physician leaders, particularly those overseeing medical groups and health plans. Additionally, we discuss strategies to improve care quality and financial performance for this important clinical activity within our institutions.
Rationale for the Annual Wellness Visit
The AWV provides an important mechanism for delivering preventive care to Medicare beneficiaries. The AWV helps identify modifiable risk factors that lead to chronic illnesses and identifies the early signs of chronic disease by supporting preventive and screening services. It also moves beyond illness care by assessing the patient’s functional status and engaging them through the health risk assessment (HRA) to manage their health and healthcare risks.(3–10)
As conceptualized, the AWV’s focus on prevention and risk factor management was thought to reduce the burden of chronic disease and potentially lead to lower healthcare costs for a significant portion of the nation’s most vulnerable population — Medicare beneficiaries.(3–10)
Essential Elements of the Annual Wellness Visit
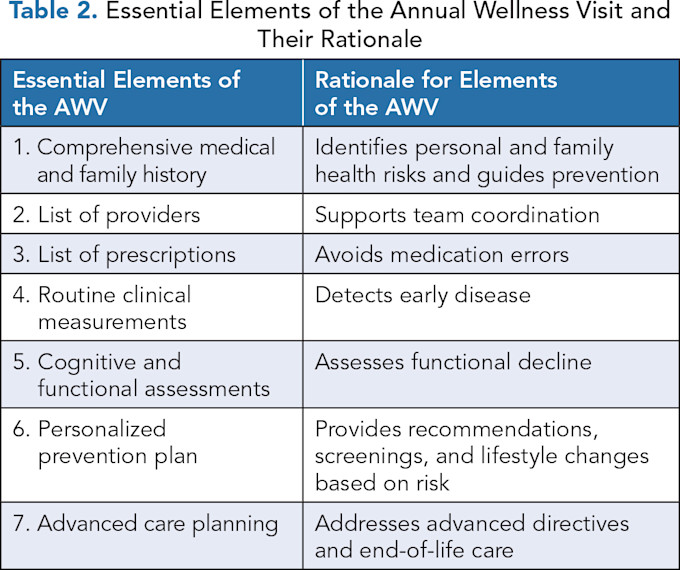
Table 2 presents the major components of the AWV and their rationale concerning providing value and ensuring billing compliance. These elements provide a comprehensive and proactive approach to improving the health of Medicare recipients.
Patient Responsibilities for the Annual Wellness Visit
The patient or their caregiver usually completes the Health Risk Assessment (HRA) to provide an important foundation for understanding their health risks through information about their demographics, at-risk behaviors, psychosocial risks, and family history.(8–12) The results help the provider generate a plan that addresses modifiable risk factors.
For example, some health behaviors, such as smoking or inactivity, can be linked to chronic diseases. Modifying these behaviors can address the occurrence and severity of these conditions, potentially lessening the impact on the patient from these diseases. Similarly, functional impairments in thought or ambulation may lead to identifying risk factors that can be addressed before a bad outcome, like a fall.
In aggregate, the HRA provides an opportunity for patient engagement and a stronger patient-provider relationship and informs an executable plan to reduce risk.(9,11)
THE ROLE OF THE PHYSICIAN LEADER AND CLINICAL TEAM
An organization’s approach to the AWV is important for ensuring the completion and compliance of these visits. Hence, the physician leader, often responsible for guiding the team in executing this work, is important in ensuring their successful completion. While the physician leader may not be directly responsible for planning and scheduling the patient or the billing, the oversight of these functions, through collaboration, teamwork, data management, and performance improvement, is essential.
Figure 1 highlights the complex steps of identifying which patients need an AWV, educating them on what the visit entails and why it’s important, and confirming its completion through proper documentation.
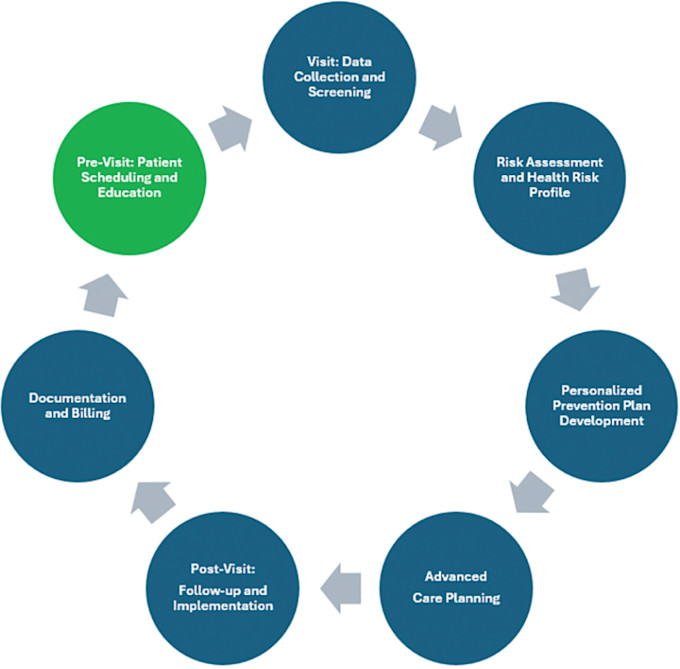
Figure 1. Process Steps Associated with the Medicare Annual Wellness Visit
Once the patient arrives in the office, team members can often participate in the patient’s care, ensuring sign-in and triage. The patients themselves can complete the HRA or be assisted by a staff member while vital signs are taken. These process steps drive efficiency in the clinic’s throughput (Figure 1).
While physicians have traditionally taken the lead in performing AWVs, other clinically trained providers, including nurse practitioners, physician assistants, pharmacists, and nurses, now augment the healthcare team and support the completion of AWVs, bringing different perspectives regarding risk assessment.(10,13–16) These efforts enhance the patient relationship, improve care continuity, and promote healthier aging; yet, most healthcare consumers prefer to have a physician as their primary care provider.(17)
Providers are responsible for reviewing the data on medical, family, and social histories, identifying risk factors, and developing prevention plans, and are central to the AWV’s success.(10) The early detection of chronic conditions allows for timely interventions that can reduce disease progression. The providers performing the AWV are also responsible for identifying and coordinating care with other members of the healthcare team, including specialists for complex health needs.(10) Their clinical expertise enables evidence-based recommendations, fostering healthier aging and improved patient outcomes. By engaging patients in long-term health planning, physicians can ensure continuity of care and reduce healthcare costs.
NATIONAL DATA AND ECONOMIC IMPLICATIONS
Completion Rates and Outcomes
Despite the 15 years since the passage of PPACA, the national completion rates for the AWV have been and remain low, with fewer than 30% of eligible Medicare beneficiaries having completed the AWV in 2021.(1,18) Reasons for this failure of performance include a lack of awareness, scheduling issues for patients, and a belief that the AWV adds little value to the patient’s care.
For example, because the AWV does not include vital signs and a physical examination, many physicians and patients may question the exam’s value. Regardless of the reasons, underutilization limits the potential for clinical improvements in Medicare patients at the population health level.
Further, data demonstrating the outcomes of the AWV are equivocal. On the one hand, beneficiaries who complete the AWV are consistently more likely to undergo preventive screenings like colonoscopy, mammography, and cardiovascular risk factor assessment, all of which can lead to early detection and improve chronic disease management.(3–8) In addition, while a modest reduction in total costs has been demonstrated,(19) emergency department visits and hospitalizations were not found to be associated with AWV completion rates.(19)
Physician Reimbursement and RVUs
The AWV may also offer economic benefits for physician groups and practices. In 2025, the Medicare Prospective Payment System projects reimbursement at $148 to $206 for initial AWVs and between $116 and $161 for subsequent AWVs, depending on service level and location.(20) A standard office visit ranges from $63 to $275 for new patients and $20 to $224 for established patients based on service level and location (Table 3).
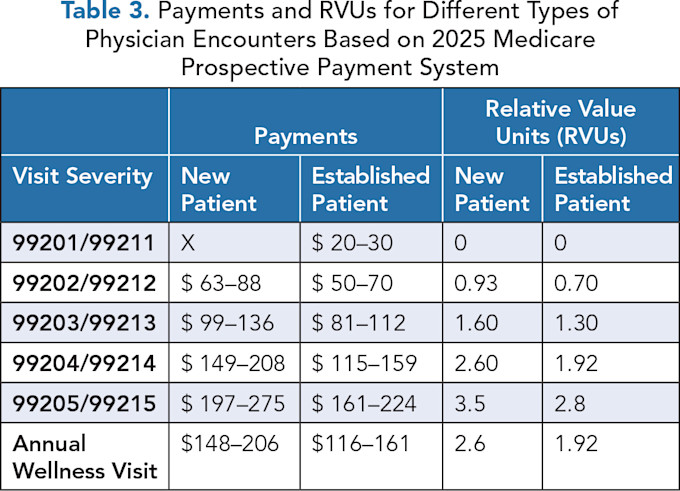
The work relative value units (wRVUs) associated with an initial and subsequent AWV are 2.6 and 1.92, respectively, and compare favorably with the wRVUs and, thereby, payment related to higher-level evaluation and management (E&M) services.(21) Despite this, some physicians may prefer to address the issues of the AWV within a traditional visit and bill E&M codes because of the complex nature of documenting the AWV.
CONSIDERATIONS FOR PHYSICIAN LEADERS AND EXECUTIVES
Enhancing clinical and financial performance through the completion of AWVs requires strategic leadership and thoughtful planning. Physician leaders and executives are essential for ensuring that AWVs are consistently offered to eligible Medicare beneficiaries and effectively integrated into clinical workflows to maximize clinical and financial performance for their organization. Three important strategies to help improve AWV completion rates and outcomes are team-based education, workflow optimization, and patient outreach.
1. Team-Based Education and Integration
First, physicians and staff should understand the AWV’s purpose, billing requirements, and documentation standards. Providing education and training to ensure that the team of providers understands the clinical and financial significance of the AWV and the specific elements for each visit, like the Health Risk Assessment (HRA), screenings, and care plan development, is essential for improving AWV completion rates. Physicians and staff also must be familiar with Medicare’s documentation standards to ensure proper billing and reimbursement. Insufficient understanding of these processes can lead to underutilization of AWVs, billing errors, and missed preventive care opportunities.(22)
Therefore, providing targeted team-based education and training is a key strategy for improving the quality and consistency of AWV delivery and ensuring that healthcare providers comply with regulatory and reimbursement requirements. This approach also minimizes administrative errors and supports efficient billing processes, ultimately enhancing financial performance for healthcare practices.
In addition, because successfully executing AWVs in an organization is a complex undertaking, a team-based approach with clearly defined roles often works well. Routine elements of an AWV, like the HRA or aspects of cognitive functioning and emotion, can be delegated to other providers to improve clinic workflow. This approach utilizes the clinical expertise of all providers and ensures a more efficient operating team.
2. Workflow Optimization and Integration
Another critical strategy for enhancing AWV completion rates is workflow optimization. Incorporating AWVs into routine care schedules and leveraging electronic health records (EHRs) for reminders and tracking can significantly improve efficiency and ensure AWVs become a standard part of clinical practice. The EHR can automate the scheduling of AWVs, send reminders to patients, and track the completion of required components, such as the HRA and preventive screenings, leading to higher rates of AWV completion.(23)
These technological solutions can streamline administrative tasks, reduce the burden on staff, and facilitate timely follow-up care, ultimately improving the delivery of AWVs and promoting better health outcomes for Medicare beneficiaries.(23) For example, improving AWV performance and compliance depends on charting all data elements consistently and completely. Using standardized documentation templates with “hard stops” for missing elements ensures complete clinical documentation and reimbursement compliance. The standardized template also provides the team with expectations and an opportunity to manage performance metrics with accountability.
In addition, given the number of chronic conditions each Medicare beneficiary has, these visits represent an important opportunity to ensure the patient has what they need for chronic disease management. These services can generate a separate E&M code and be reimbursed separately, even when performed in the same visit with appropriate documentation.
3. Patient Outreach
Effective communication strategies to educate patients about the AWV’s significance, purpose, and benefits can improve engagement and outcomes. By implementing targeted patient outreach efforts, healthcare organizations can inform beneficiaries about the preventive services available through the AWV, such as screenings for cancer, cardiovascular disease, and diabetes, and the importance of creating a personalized prevention plan. Proactive outreach efforts, such as phone calls, mailed reminders, and educational materials, increase patient awareness and participation in wellness visits.(24)
In addition, outreach can address common barriers such as transportation issues, lack of time, or misconceptions about the visit. Through tailored communication that emphasizes the personal health benefits and long-term value of AWVs, healthcare organizations can enhance patient engagement and improve completion rates. Importantly, patient-centered approaches to outreach should consider the unique needs of diverse populations, ensuring all eligible beneficiaries are informed and encouraged to participate in these vital preventive care services.
Physician leaders and healthcare executives can improve AWV completion rates by focusing on three main areas: education and training, workflow optimization, and patient outreach. By adopting these strategies, the quality of care and financial sustainability of the practices can be improved, ultimately contributing to the broader goals of preventive healthcare and cost reduction for patients insured by Medicare. In addition, each subsequent visit represents a new opportunity to engage, motivate, and discuss chronic disease prevention and management with Medicare recipients.
MONITORING METRICS
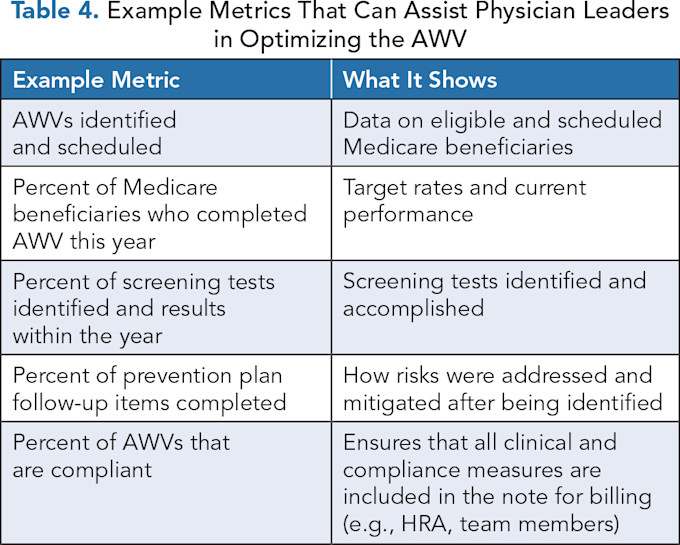
Physician leaders recognize the importance of using data to drive and manage improvement efforts, allowing them to identify those areas that meet performance expectations and those that require enhancement. Monitoring performance metrics is important for ensuring an organization’s AWV completion and compliance rates are improving.
Table 4 provides some examples of metrics that can be helpful for physician leaders who are managing AWV programs. Insights gained from these data can inform a continuous quality improvement approach that helps to drive improvements in clinical, operational, and financial performance related to AWVs.
CONCLUSION
Fifteen years ago, the Medicare Annual Wellness Visit (AWV) was conceptualized as an important preventive strategy for older adults to address health risks and promote long-term well-being. The AWV allows providers and patients to partner in identifying these health risks and organizing them into an individualized health improvement plan that can be renewed annually.
National AWV completion rates are low despite positive outcomes in prevention and being associated with total costs of care comparable to other Medicare Physician Fee Schedule (MFFS) services. Physician leaders have an important role in emphasizing the completion of the AWV as a comprehensive and proactive approach to improve healthcare outcomes of older adults, reduce their total costs of care, and support sustainable care practices.
Further, as physician leaders often have direct oversight of the clinical, operational, and financial outcomes of the AWV, which are frequently substantial for healthcare organizations, it is incumbent upon them to not merely analyze the mistakes of the past but rather strategize new ways to improve patient participation, thereby enhancing patient satisfaction and outcomes.
References
Centers for Medicare & Medicaid Services. Medicare Monthly Enrollment. Data.cms.gov. Accessed January 1, 2025. https://data.cms.gov/summary-statistics-on-beneficiary-enrollment/medicare-and-medicaid-reports/medicare-monthly-enrollment?utm_source .
Mehta N, Jha S. The Patient Protection and Affordable Care Act in a Nutshell. J Amer College Radiol. 2012;9(12):877–880. https://doi.org/10.1016/j.jacr.2012.09.009
Camacho F, Yao NA, Anderson R. The Effectiveness of Medicare Wellness Visits in Accessing Preventive Screening. J Prim Care Community Health. 2017;8(4):247–255. doi: 10.1177/2150131917736613.
Maciosek MV, Coffield AB, Flottemesch TJ, Edwards NM, Solberg LI. Greater Use of Preventive Services in U.S. Health Care Could Save Lives at Little or No Cost. Health Aff (Millwood). 2010;29(9):1656–1660. doi:10.1377/hlthaff.2008.0701
Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of Chronic Disease in the 21st Century: Elimination of the Leading Preventable Causes of Premature Death and Disability in the USA. Lancet. 2014;384(9937):45–52. doi:10.1016/S0140-6736(14)60648-6
Jiang M, Hughes DR, Wang W. The Effect of Medicare’s Annual Wellness Visit on Preventive Care for the Elderly. Prev Med. 2018;116:126–133. https://doi.org/10.1016/j.ypmed.2018.08.035
Odden MC, Coxson PG, Moran A, Lightwood JM, Goldman L, Bibbins-Domingo K. The Impact of the Aging Population on Coronary Heart Disease in the United States. Am J Med. 2011;124(9):827–833.e5. doi:10.1016/j.amjmed.2011.04.010
Ganguli I, Souza J, McWilliams JM, Mehrotra A. Association of Medicare’s Annual Wellness Visit with Cancer Screening, Referrals, Utilization, and Spending. Health Aff (Millwood). 2019;38(11):1927–1935. doi: 10.1377/hlthaff.2019.00304
Powell DS, Wu MMJ, Nothelle S, Gleason K, Oh E, et al. The Annual Wellness Visit Health Risk Assessment: Potential of Patient Portal-Based Completion and Patient-Oriented Education and Support. Innov Aging. 2024;8(3):igae023. doi:10.1093/geroni/igae023
Passmore RC, Iqbal A, Rader TL, Ashley K, Canoy AJ, Madden KA, et al. Team-Based Approach to Successful Annual Wellness Visits. J Prim Care Community Health. 2024;15:21501319241249400. doi:10.1177 /21501319241249400
Nothelle SK, McGuire M, Boyd CM, Colburn JL, Stephanie Nothelle CK. Effects of Screening for Geriatric Conditions and Advance Care Planning at the Medicare Annual Wellness Visit. J Am Geriatr Soc. 2022;70:579–584. https://doi.org/10.1111/jgs.17546
Misra A, Lloyd JT, Strawbridge LM, Wensky SG. Use of Welcome to Medicare Visits Among Older Adults Following the Affordable Care Act. Am J Prev Med. 2018;54(1):37–43. https://doi.org/10.1016/j.amepre.2017.08.030
Sewell MJ, Riche DM, Fleming JW, Malinowski SS, Jackson RT. Comparison of Pharmacist and Physician Managed Annual Medicare Wellness Services. J Manag Care Spec Pharm. 2016;22(12):1412–1416. doi:10.18553/jmcp.2016.22.12.1412
Warshany K, Sherrill CH, Cavanaugh J, Ives TJ, Shilliday BB. Medicare Annual Wellness Visits Conducted by a Pharmacist in an Internal Medicine Clinic. Am J Health Syst Pharm. 2014;7:44–49. doi:10.2146/ajhp130202
Woodall T, Landis SE, Galvin SL, Plaut T, Roth McClurg MT. Provision of Annual Wellness Visits with Comprehensive Medication Management by a Clinical Pharmacist Practitioner. Am J Health Syst Pharm. 2017;74(4):218–223. doi:10.2146/ajhp150938
Tetuan TM, Ohm R, Herynk MH, Ebberts M, Wendling T, Mosier MC. The Affordable Health Care Act Annual Wellness Visits: The Effectiveness of a Nurse-Run Clinic in Promoting Adherence to Mammogram and Colonoscopy Recommendations. J Nurs Adm. 2014;44(5):270–275. doi:10.1097/NNA.0000000000000066
Dill MJ, Pankow S, Erikson C, Shipman S. Survey Shows Consumers Open to a Greater Role for Physician Assistants and Nurse Practitioners. Health Aff (Millwood). 2013;32(6):1135–1142. doi:10.1377/hlthaff.2012.1150
Ganguli I, Souza J, McWilliams JM, Mehrotra A. Trends in Use of the US Medicare Annual Wellness Visit, 2011–2014. JAMA. 2017;317(21): 2233–2235. https://doi.org/10.1001/jama.2017.4342
Beckman AL, Becerra AZ, Marcus A, et al. Medicare Annual Wellness Visit Association with Healthcare Quality and Costs. Am J Manag Care. 2019;25(3):e76-e82.
Centers for Medicare and Medicaid Services. Physician Fee Schedule. Accessed January 30, 2025. https://www.cms.gov/medicare/physician-fee-schedule/search?Y=1&T=4&HT=0&CT=3&H1=G0439&M=5 .
AAPC. Work RVU Calculator (Relative Value Units). AAPC Tools. Accessed January 30, 2025. www.aapc.com/tools/rvu-calculator.aspx .
Taylor EF, Machta RM, Meyers DS, Genevro J, Peikes DN. Enhancing the Primary Care Team to Provide Redesigned Care: The Roles of Practice Facilitators and Care Managers. Ann Fam Med. 2013;11(1):80–83. doi:10.1370/afm.1462
Adler-Milstein J, Embi PJ, Middleton B, Sarkar IN, Smith J. Crossing the Health IT Chasm: Considerations and Policy Recommendations to Overcome Current Challenges and Enable Value-Based Care. J Am Med Inform Assoc. 2017;24(5):1036–1043. doi:10.1093/jamia/ocx017
Kaplan RS, Anderson SR. Time Driven Activity Based Costing. Harvard Business Review. November 2004. Accessed January 27, 2025. https://hbr.org/2004/11/time-driven-activity-based-costing .

